COMPASS BLOG
Bone Healing:
What to Expect as you Heal After a Fracture
Sarah Wilcox - 9 September 2025
A few weeks ago, my son broke his femur and we've spent quite a bit of time discussing the recovery process, so he could understand what his body was doing while it healed (and to get him to fully understand why he can't get back to his full sport schedule as soon as he'd like). In doing this, I realised that many people have the same questions about how bone healing really works....
Your body is smarter than you think. Break a bone and without you even asking, it launches a full repair team to put things back together. Pretty amazing, right? When a bone breaks, the body starts a natural, step-by-step process to repair itself. Healing happens in stages and each stage has an important role in restoring strength, movement and function.
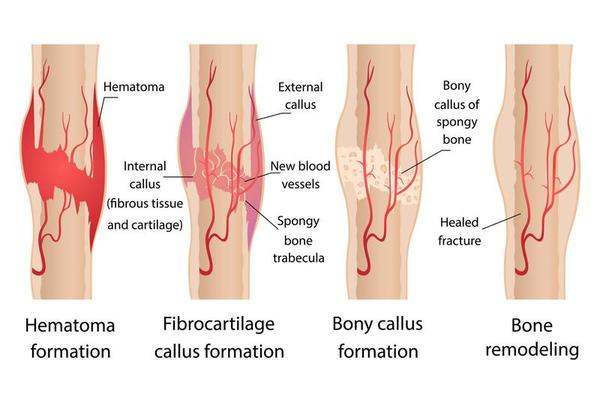
1. Haematoma Formation (First Few Days).
Immediately after the break, blood collects around the fracture
(haematoma); this also triggers an inflammatory response that peaks within the
first 48 hours. Immune cells rush in to clear debris and prepare the area for
the upcoming healing process. During this stage, swelling, bruising, and pain
are completely normal. No new bone is visible on X-rays yet, but this early step is
essential for setting the foundation for recovery. Immobilisation of the bone itself is important
at this stage to protect the bone, this can be in the form of a cast, splint or surgical fixation. Depending on consultant/surgeon/health department, gentle acute PT-led movement may be
initiated once the immediate trauma has subsided, to ensure the joints above and
below the fracture site maintain range.
2. Soft Callus Formation (1-3 Weeks).
As the initial swelling goes down, the body starts to form a
soft callus, a temporary bridge of tissue that connects the broken ends of
the bone. Chondroblasts (specialised cells) produce cartilage, which act like
a flexible filler to help stabilise the fracture site while it heals; this is one of the most
vital components of bone healing. While it’s not yet hard bone, this scaffold supports the fracture as well as facilitates the ongoing cellular activity that is involved with the healing process. Further gentle, guided movement may begin depending on your fracture and your clinician’s advice, helping maintain joint range and muscle length.
3. Hard Callus and Calcification (3-6 Weeks).
Bone-building cells, called osteoblasts, start laying down
minerals (mainly calcium phosphate) into the callus. This process hardens it
and transforms it into new, woven bone; hard callus that shows on X-rays. The
bone is stronger but still immature, without the structural organisation of bone,
so activity must remain controlled to prevent disruption of the healing site.
At this stage, introducing weight-bearing and mechanical stress, under guidance, helps the bone adapt and become stronger (Wolff's law). Depending on your fracture and treatment plan, the cast or splint may be removed toward the end of this stage, allowing you to begin more active physical therapy. Removal or surgical fixation may, or may, not be removed further down the line but this is on a patient-by-patient basis.
4. Bone Remodelling (6 Weeks to Several Months.
The final stage refines the bone into its original shape and strength. The hard callus formed earlier is gradually replaced with stronger, ‘lamellar’ bone. Osteoclasts (bone absorbing cells) remove excess bone, whilst osteoblasts continue with their task of rebuilding it according to your body’s needs. Rehabilitation becomes more active here: weight-bearing exercises, resistance training and mobility work restore joint range, muscle length, and confidence in movement. Return to performance specific levels of activity will require further input and a graded exposure to the intensity, volume and loading that an individual may have undertaken before.
How will my lifestyle effect my healing?
Factors such as your age, bone density, and lifestyle can significantly influence how long the remodelling phase takes, largely because they affect the activity of the bone cells driving the process. In younger people, osteoblasts are generally more active, which means new bone is laid down more quickly. In contrast, with age or reduced bone density, these cells work more slowly, and osteoclasts may become more dominant, making repair less efficient.
Lifestyle choices also directly affect cellular activity. For example, smoking reduces blood flow to the healing area and lowers the oxygen supply that bone cells need to function, which can suppress osteoblast activity and delay new bone formation. Poor nutrition, particularly low calcium or vitamin D, can deprive osteoblasts of the raw materials they need to build strong bone. On the other hand, good habits, like a balanced diet, regular weight-bearing exercise and avoiding excessive alcohol, support healthy cellular function, helping osteoblasts and osteoclasts work together effectively to remodel bone.
How Compass Performance Can Help?
Physicial therapy or physiotherapy usually guides you through the early stages of bone healing, reducing swelling, restoring safe movement and building a base of strength. Once you’ve been signed off by your physical therapist, that’s where Compass Performance steps in. Through guided, physio-influenced, evidence-based approaches, my focus is on taking your recovery further. With a blend of strength training, mobility, function-specific progression along with education, I help you rebuild confidence, resilience and long-term strength so you can return not just to activity, but to moving at your best.
** This information is provided for educational purposes only
and is not intended as medical advice. It should not replace the guidance of
your physician, physical therapist, or other licensed healthcare provider.
Always follow the recommendations of your medical team and consult them before
making changes to your rehabilitation or exercise program. **
References:
Chang, C.-J., Jou, I-Ming., Wu, T.-T., Su, F.-C. and Tai, T.-W. (2020). Cigarette smoke inhalation impairs angiogenesis in early bone healing processes and delays fracture union. Bone & Joint Research, [online] 9(3), pp.99–107. doi:https://doi.org/10.1302/2046-3758.93.bjr-2019-0089.r1.
Langdahl, B., Ferrari, S. and Dempster, D.W. (2016). Bone modeling and remodeling: potential as therapeutic targets for the treatment of osteoporosis. Therapeutic Advances in Musculoskeletal Disease, [online] 8(6), pp.225–235. doi:https://doi.org/10.1177/1759720x16670154.
Lu, Y., Di, Y.P., Chang, M., Huang, X., Chen, Q., Hong, N., Kahkonen, B.A., Di, M.E., Yu, C., Keller, E.T. and Zhang, J. (2021). Cigarette smoke-associated inflammation impairs bone remodeling through NFκB activation. Journal of Translational Medicine, [online] 19(1). doi:https://doi.org/10.1186/s12967-021-02836-z.
Marsell, R. and Einhorn, T.A. (2011). The Biology of Fracture Healing. Injury, [online] 42(6), pp.551–555. doi:https://doi.org/10.1016/j.injury.2011.03.031.
Rowe, P., Koller, A. and Sharma, S. (2023). Physiology, bone remodeling. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK499863/ [Accessed 6 Sep. 2025].
Sheen, J.R., Garla, V.V. and Mabrouk, A. (2023). Fracture healing overview. [online] National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK551678/ [Accessed 7 Sep. 2025].
Image: https://www.shutterstock.com/g/natun/
Disclaimer:
The content on this blog is for informational purposes only and is not intended to provide medical advice, diagnosis, or treatment. Always consult your physician or a qualified healthcare provider if you have concerns about your health or specific medical conditions.
